PATIENTS: Please visit National Accreta Foundation’s Patient & Family Resources page for a patient facing FAQ based on the latest literature and evidence based care recommendations for women with placenta accreta.
PROVIDERS: Please visit National Accreta Foundation’s Professional Resources page for the latest in professional society publications related to placenta accreta.
Obstetric Care Consensus No. 7 on Placenta Accreta Spectrum was released jointly by The American College of Obstetricians and Gynecologists and Society for Maternal-Fetal Medicine in December 2018 and replaced ACOG Committee Opinion No. 529. The article below was written in 2017 and has not yet been updated to reflect new data where available.
Minimizing the risk of placenta accreta complications at your hospital
By Jill Arnold
November 10, 2017
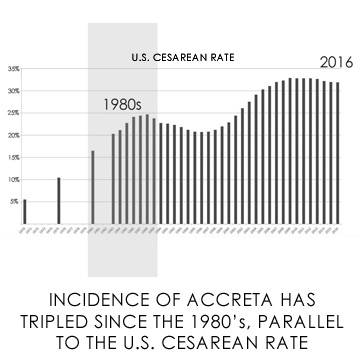
The estimated incidence of placenta accreta has tripled since the 1980's and has risen parallel to the cesarean rate. [1] An estimated 7% of women with placenta accreta die, usually due to hemorrhage. Up to 90% of accreta patients require a blood transfusion, with an average blood loss of 3000 to 5000mL. [2] A history of placenta accreta is an independent risk factor for postpartum hemorrhage, as is a history of prior cesarean birth. [3]
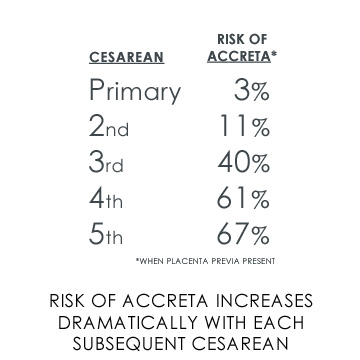
Women with multiple cesareans are at an increased risk for placenta accreta with each subsequent cesarean birth, especially in the presence of placenta previa. [1] The current ACOG Committee on Practice Bulletins- Obstetrics affirmed the dose–response relationship between placenta accreta and number of previous cesareans in the newly revised Vaginal Birth After Cesarean Delivery Practice Bulletin. [4]
ACOG Committee Opinion on Placenta Accreta provides a review of literature on diagnosis and management of placenta accreta. Undiagnosed placental abnormalities can present a challenge to small and rural facilities without adequate blood supplies on hand or access to subspecialists required for a complicated accreta delivery. [2]
Early diagnosis of abnormal placentation and established protocols for transfer to a tertiary care center minimize potential risk by allowing for multidisciplinary planning for delivery at a risk-appropriate facility. [2] Telemedicine consultations with a centralized team of maternal-fetal medicine specialists can aid small hospitals in the management of suspected placenta accreta cases throughout the pregnancy. [5]
In addition to patient counseling prior to and during their childbearing years on maintaining a healthy lifestyle, including smoking cessation and weight management, as well as family planning and pregnancy spacing, there are practice modifications and patient safety bundles that will minimize risk of maternal and neonatal morbidity and mortality from placenta accreta.
Decisions made regarding cesarean birth in a woman's first pregnancy will likely affect the rest of her reproductive life. For this reason, both ACOG and Society for Maternal Fetal Medicine (SMFM) recommend safe reduction of primary cesarean utilization.[6] Additionally, for patients with history of prior cesarean, ACOG recently announced that it no longer recommends that a physician be "immediately available" for TOLAC, and that candidates can undergo TOLAC in any hospital that provides access to emergency cesarean sections. [4]
Resources for Preventing Accreta and Managing Obstetric Hemorrhage
Both ACOG and SMFM, along with 20 other professional organizations and patient advocates, comprise the Council on Patient Safety in Women's Health Care. The implementation arm of the Council, Alliance for Innovation on Maternal Health (AIM), provides implementation support and data tracking for patient safety bundles.
ACOG Committee Opinion on Placenta Accreta
SMFM Clinical Guidelines on Placenta Accreta
ACOG/SMFM Levels of Maternal Care
ACOG/SMFM Safe Prevention of the Primary Cesarean Delivery
South Central Telehealth Resource Center (serves Arkansas, Mississippi and Tennessee)
Five Steps Hospitals Can Take to Safely Lower Their Cesarean Rate
Belfort, M.A. Placenta accreta. Am J Obstet Gynecol 2010; 203:430-439.
Placenta accreta. Committee Opinion No. 529. American College of Obstetricians and Gynecologists. Obstet Gynecol 2012;120:207–11.
Vinograd, A. A prior placenta accreta is an independent risk factor for post-partum hemorrhage in subsequent gestations. Eur J Obstet Gynecol Reprod Biol. 2015;187:20–24.
Vaginal Birth After Cesarean Delivery. Practice Bulletin No. 184. American College of Obstetricians and Gynecologists. Obstet Gynecol 2017;130:e217-e233.
Health Disparities in Rural Women, Committee Opinion No. 586. American College of Obstetricians and Gynecologists. Obstet Gynecol 2014;123:384-8.
Caughey, A.B. Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol 2014; 210:179–193.


